Leslie Russek, Clarkson University
Connective tissue is found throughout the human body, within and between structures as varied as muscles, nerves and internal organs. Like an elaborate web, it holds everything together – providing the body shape and promoting proper movement.
Many people, especially young women, have very flexible connective tissue. While flexibility is essential for childbirth – and an advantage to dancers and gymnasts – fragile and stretchy connective tissue can sometimes lead to a variety of health problems.
Overly mobile joints are prone to injuries like sprained ankles, dislocated shoulders and chronic neck pain. Hypermobile connective tissue can also cause serious health problems throughout the body, including the gut, nerves, skin, urinary tract and even immune system.
Many health care providers, especially in the U.S., have not been trained to look for problems related to hypermobility, which means it often takes people with hypermobile connective tissue disorders a decade or more to be diagnosed. Although many clinicians were taught that connective tissue disorders are rare, current estimates suggest that as much as 2% of the overall population experiences symptoms related to hypermobility, and around a third of people treated in pain management or rheumatology clinics may be hypermobile.
I’m a physical therapist and researcher who specializes in treating conditions arising from hypermobility. When I tell patients their years of symptoms are real, can be explained and are potentially manageable, some have cried with relief.
Wide range of symptoms
Symptomatic generalized joint hypermobility is the most inclusive term for conditions caused by hypermobile connective tissue. While some forms have genetic markers, more than 90% of hypermobility conditions – including hypermobile Ehlers-Danlos syndrome and hypermobility spectrum disorder – do not. They are diagnosed by a physical exam using a diagnostic checklist. Symptoms and severity can differ greatly from person to person and vary over time.
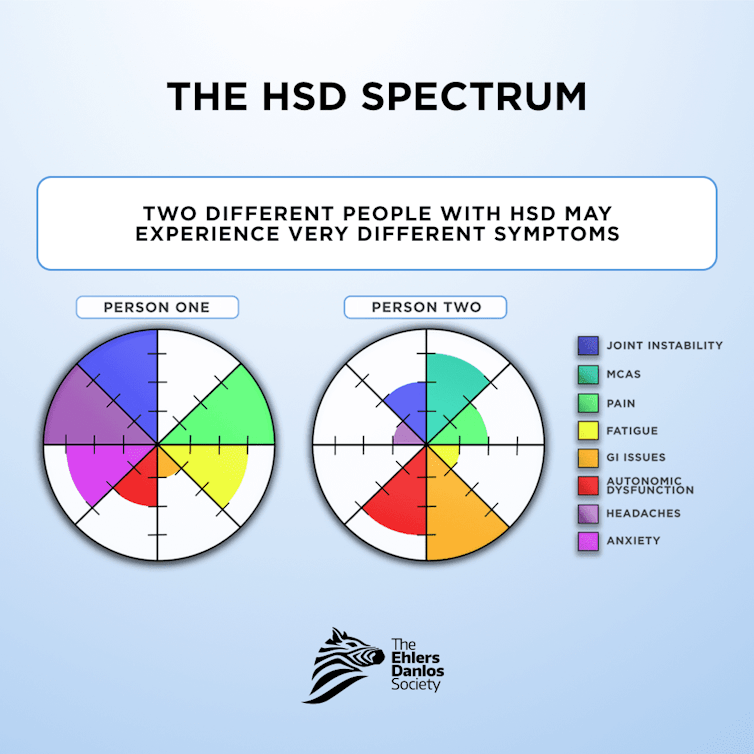
Symptoms can include widespread pain and frequent injury, irritable bowel syndrome, indigestion, hernias, frequent bruising and poor skin healing, trouble breathing, migraines and headaches, dizziness, fatigue, insomnia, anxiety and trouble concentrating.
Some of these problems are purely mechanical, such as fragile skin that tears easily and heals poorly, stretchy gut tissue that doesn’t move along digesting food as quickly as it should and excessive mobility between the skull and top vertebra that can compress the brain stem and lead to central nervous system problems.
Additionally, people with hypermobility conditions have problems that scientists don’t yet understand. For example, the autonomic nervous system – which regulates functions like digestion, breathing and heart rate – is out of balance. Similarly, research has not fully explained the connection between hypermobility and mast cells, which are part of the immune system protecting against viruses and other invaders. One hypothesis is that overactive mast cells may release chemicals affecting surrounding connective tissue.
Often, multiple factors contribute to a given symptom. For example, the problem of insomnia is due, in part, to pain that keeps people awake. But lax tissue in the throat can cause sleep apnea, as well. What’s more, an overactive nervous system and anxiety about unexplained health issues can also lead to poor sleep.
Ehlers-Danlos syndrome is the most common heritable connective tissue disorder. It was first described by Hippocrates in 400 BCE but was formally defined by doctors Edvard Ehlers and Henri-Alexandre Danlos in the early 1900s. About 90% of all Ehlers-Danlos patients have the hypermobile type.
Doctors have traditionally considered hypermobile Ehlers-Danlos syndrome a rare condition, which is how people with hypermobility came to be called zebras. Medical students are taught, “When you hear hoofbeats, look for horses, not zebras,” as a reminder that rare conditions are seldom seen, and virtually all hoofbeats indicate horses. Hypermobility experts now believe Ehlers-Danlos syndrome is not as rare as previously thought – and many people are misdiagnosed or undiagnosed.
Difficulties with diagnosis
Lack of a diagnosis can be frightening and discouraging for people with hypermobility spectrum disorder. Patients are often told nothing is wrong with them and they are just complaining too much or have low pain tolerance. Many may be considered difficult patients, because they see multiple health care providers trying to understand their symptoms – and often present with complaints that vary from day to day.
Some providers believe their patients but simply do not know how to manage their problems. Other patients report being subjected to medical gaslighting, being told repeatedly, “It’s all in your head.” Women are more likely to be told that their problems are psychiatric rather than physiologic. Hypermobile patients frequently feel abandoned by the health care system.
Even once diagnosed, hypermobile patients often struggle to find knowledgeable providers who can help rather than make problems worse. A 2022 study showed only 9% of physicians were familiar with the diagnostic criteria for hypermobile Ehlers-Danlos syndrome – and only 4% reported feeling comfortable treating it.
Failure to diagnose underlying hypermobility can lead to inappropriate treatments, such as unhelpful medications, surgeries that might be less effective for hypermobile patients or even inappropriate psychiatric diagnoses. A delayed diagnosis leads to worse function, increased pain and disability.
How physical therapy can help hypermobility
There is no cure for the actual connective tissue abnormality. So, treatment strives to minimize pain and injury while improving joint stability, overall health and daily function.

Joints normally provide sensory information about where the body is in space, but this system does not function properly in hypermobile people, who often do not realize joints are moving in ways they should not. Although research is limited, existing research suggests that physical therapy can improve sensory awareness and motor control – and help patients identify, activate and strengthen stabilizing muscles.
Since many hypermobile patients have sensitive nervous systems, systemic calming is an important part of pain relief. Patient education, movement, sleep, mind-body training and nutrition can also help manage pain with minimal medication.
Occupational therapy can also benefit hypermobile patients through environmental modifications, activity pacing and assistive and mobility devices like splints, braces and wheelchairs.
Other management approaches include nutrition, psychosocial support and medical management through medications and surgery. Orthopedic surgeries appear to be less successful in hypermobile people compared with nonhypermobile people, so nonsurgical options should be explored before considering surgery.
Symptomatic generalized joint hypermobility is a complicated condition that is not yet fully understood. Once it has been identified, though, many strategies can help decrease pain and injuries – and improve function and quality of life.
Leslie Russek, Professor Emeritus of Physical Therapy, Clarkson University
This article is republished from The Conversation under a Creative Commons license. Read the original article.






